For people with moderate-to-severe asthma, personalization of biologic agents is warranted based on factors such as biomarkers and comorbidities. PlatformQ Health and the Asthma and Allergy Foundation of America (AAFA) conducted a CME-certified, case based, expert panel discussion that featured a live Q&A session with leading faculty from the Asthma Center at Cincinnati Children’s Hospital Medical Center and the Division of Allergy and Immunology at Northwestern University’s Feinberg School of Medicine, as well as AAFA’s public health manager. Four short educational video excerpts from the session were also shared on LinkedIn to reach NPI-verified pulmonologists.
PlatformQ Health then conducted an assessment to determine the affect of the education on adoption of personalized biologic treatment among pulmonologists and allergists/immunologists. We shared the results in a poster session at the 2024 American Thoracic Society (ATS) conference.
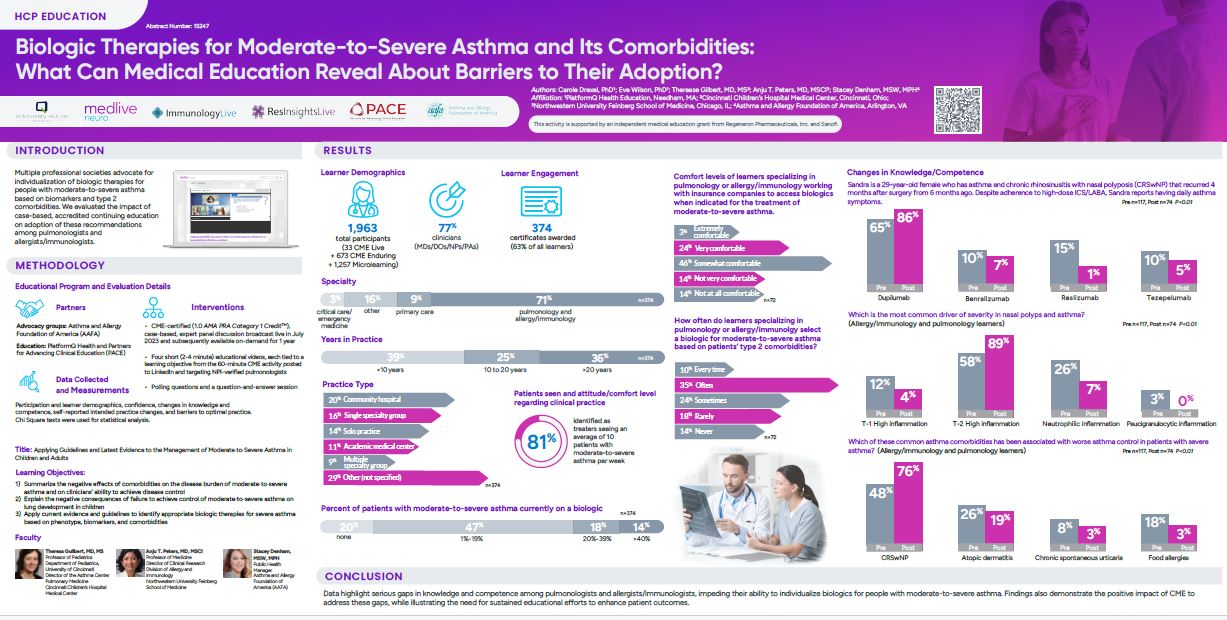
673 learners attended the CME session and 1,257 watched the “microlearning” (video excerpt) sessions. 71% of learners identified as specializing in pulmonology, allergy, or immunology, while 9% work in primary care, 3% in critical care/emergency medicine, and 16% work in other areas. They come from diverse settings, including academic medical centers, multiple specialty groups, and solo practices. 81% identified as treating an average of 10 patients with moderate-to-severe asthma per week.
Prior to the session, nearly half reported that only 1-19% of their patients with moderate-to-severe asthma were currently on a biologic. Notably, only 25% reported being very comfortable working with insurance companies to access biologics when indicated.18% said they rarely select a biologic and 14% said they never do.
Through patient case studies, the CME session educated specialists about the negative effects of comorbidities on disease burden and disease control, the challenges in achieving control of moderate-to-severe asthma on lung development and children, and the application of current evidence to identify appropriate biologic therapies based on phenotype, biomarkers, and comorbidities.
Pre- and post-session surveys demonstrated an improvement in specialist knowledge and competencies across these areas. The data also identified notable knowledge gaps that necessitate sustained educational efforts to improve patient outcomes.