
He lay there in the ICU bed with his family standing by in the waiting area. As the intern on call, I was called to his bedside once again because his blood pressure plunged dangerously low. Unfortunately, his prognosis was poor, in fact terminal. The medical team knew this would be the last time he would be admitted to the hospital, one of many admissions, and that he would die in the hospital. His family, despite his DNR (Do Not Resuscitate) status, held out resistance and frequent family feuds broke out in the hospital among his large extended family. Looking at him, he was flushed as was typical of his untypical disease. I adjusted his fluids but carefully because his kidneys were starting to fail. In the middle of the night, I was again called to his bedside because his heart went into a dysrhythmia and since he was DNR, I could only watch the monitor until it went flat-line. An hour later, I pronounced him dead and listened to his family wail when they were told the news. He was the first patient that died on my watch. Over several months, I watched the ravages Carcinoid Syndrome took on his body over numerous hospital admissions.
Carcinoid tumor was first described in 1888 by Lubarsch and first called karzinoide tumoren (Carcinoid) in 1907 by Orbendorfer. In 1952, Erspamer and Asero identified the fact that these tumors produce serotonin. In 1980, the WHO applied the term Carcinoid to all tumors of the diffuse endocrine system.
Carcinoid tumors are one type of NeuroEndocrineTumors (NETs), or tumors that produce hormones. These tumors have the ability to produce peptides that cause the characteristic syndrome. Carcinoids are the most frequent type of NETs and can be either benign or malignant. They occur in multiple locations throughout the body.
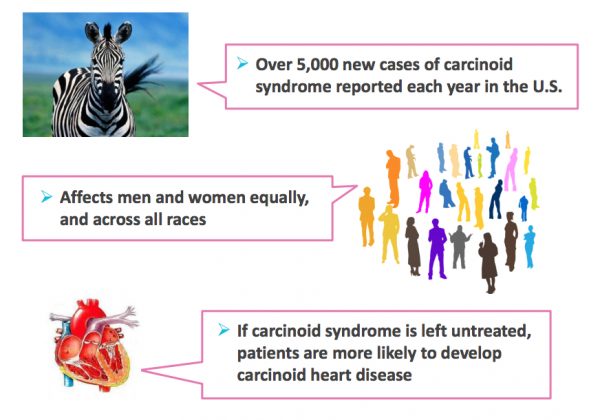
In the US, approximately 12,000 people are diagnosed with carcinoid tumor every year. The incidence appears to be rising but no one is sure why. The most common locations of carcinoid tumors appear to be in the GI tract or lungs. In the GI tract, the most common location for the development of carcinoid tumors is the small intestine. For tumors in the GI tract that have not spread to other locations, the 5 year survival is estimated to be 65-90%. For tumor that has spread locally, the 5 year survival rate is 46-78% while for disease that has spread distantly it is 14-54%. In comparison, the 5 year survival for typical pulmonary carcinoma is 85-95% while for atypical pulmonary carcinoid tumor it is 50-70%.
Carcinoid syndrome occurs when a carcinoid tumor starts secreting hormones, mostly serotonin and kallikrein into the blood stream. It usually occurs in more advanced tumors.
What are the symptoms of Carcinoid Syndrome?
- Skin flushing
- Facial skin lesions
- Diarrhea
- Wheezing and shortness of breath
- Rapid heartbeat
GI carcinoid tumors can additionally cause obstruction and abdominal pain, intestinal bleeding, Pellagra and melena. Pulmonary carcinoid tumors can also cause cough and post-obstructive pneumonia.
Other symptoms of carcinoid syndrome include heart murmur, unexplained weight gain, weakness, secondary diabetes, hirsuitism, fluctuations in blood pressure and neurosis/psychosis.
Carcinoid crisis is a life-threatening condition that occurs when a large amount of hormones are suddenly released from a carcinoid tumor. It can be triggered by manipulation of the tumor, such as happens during biopsy or surgery, or by anesthesia. Carcinoid crisis can resemble an acute allergic reaction. Signs of the crisis include sudden changes in blood pressure, rapid heart rate, wheezing, difficulty breathing, flushing and high body temperature.

Diagnosis can sometimes be difficult in the early stages because the symptoms are non-specific. Two symptoms that may be more specific for Carcinoid syndrome include dry flushing and nocturnal diarrhea. Chromogranin A (CgA testing) is a good marker to detect and follow the activity of a carcinoid tumor. It is also useful in Carcinoid syndrome. Elevated levels of CgA are found in 80-100% of patients with carcinoid tumor. However, elevated levels may also be seen in renal failure, atrophic gastritis, or the use of proton pump inhibitors. Food consumption can alter the results so patients are expected to fast prior to doing this test. A more specific test is the 5-Hydroxyindoleacetic Acid (5-HIAA) test. It is not elevated in other types of tumors. This is a by-product of the breakdown of serotonin. It identifies carcinoid tumor 75% of the time but it is only elevated when liver metastases are present. It is a 24 hour urine test but several medications, such as those found in cough and cold medications, can also cause elevations.
Imaging tests used to aid diagnosis of carcinoid tumor:
- Colonoscopy
- EGD
- Endoscopic ultrasound
- CT scan
- MRI
- Octreotide scan or somatostatin receptor scintigraphy (OctreoScan): this is the most commonly used to diagnose carcinoid tumor
- Angiogram
- Barium swallow/enema
- Enteroclysis
- I-131 MIBG scan
- Capsule endoscopy
- Double balloon enteroscopy
- Proctoscopy
Biopsy also plays an important role in establishing the diagnosis.
Treatment of carcinoid syndrome aims at controlling hormone related symptoms. Interferons and octreoide are beneficial in approximately 40% of patients. Anti-histamines additionally be useful as well as anti-diarrheal meds. Serotonin antagonists should also be given to control diarrhea and malabsorption. Corticosteroids may be helpful in carcinoid crisis. Somatostatin analogs octreotide and lanreotide are used to control symptoms and disease progression in patients with inoperable disease. Radiotherapy and/or chemotherapy also show some benefit. The best treatment, however, is complete surgical removal of all tumor tissue.
Newer treatments include targeted radionuclide therapy which is utilized for those who are not surgical candidate or have tumor that has spread. It uses 2 different substances mainly, MIBG and octreotide, to target only the carcinoid cells while leaving other cells unaffected. These substances carry the radiation to the tumor cells killing them. It must be determined before hand that the specific tumor is responsive to these substances. A newer targeted radionuclide treatment uses beads coated with radioactive yttrium-90. These beads are injected into the vessels that feed the carcinoid tumors in the liver, blocking the blood vessels and killing the tumor cells.
There are currently two promising on-going studies occurring: NETTER-1 and RADIANT-4. NETTER-1 is a phase 3 study looking at a new medication, Lutetium, while RADIANT-4 (also a phase 3 study) is investigating the targeted therapy, everolimus. There are also several studies underway exploring palliative care and increasing control of symptoms.
Other studies are exploring angiogenesis inhibitors. These targeted drugs affect the growth of new blood vessels that tumors require for growth. Some of these agents are used for other types of tumors and are now being studied for use in carcinoid tumors. Some of these include: bevacizumab, pazopanib, axitinib, and cabozantinib. Other researchers are trying to make improvements on the drug class, somatostatins. An example is pasireotide, which may prove to be more potent than existing medications in this class. Several other medications are currently in clinical trials.
Carcinoid syndrome is a rare yet deadly cancer. Patients suffer not just the effects of the tumor, but the symptoms related to the release of hormones. It is imperative that clinicians recognize this disorder. Patients and those caring for them should know as much as they can about this disorder as well.
—
If you’re treating patients with neuroendocrine tumors, please invite them to this free program that we created in partnership with the Carcinoid Cancer Foundation.
About the Author
Linda Girgis MD, FAAFP is a family physician practicing in South River, New Jersey. She was voted one of the top 5 healthcare bloggers in 2016. Follow her on twitter @DrLindaMD.

